Atrial Fibrillation
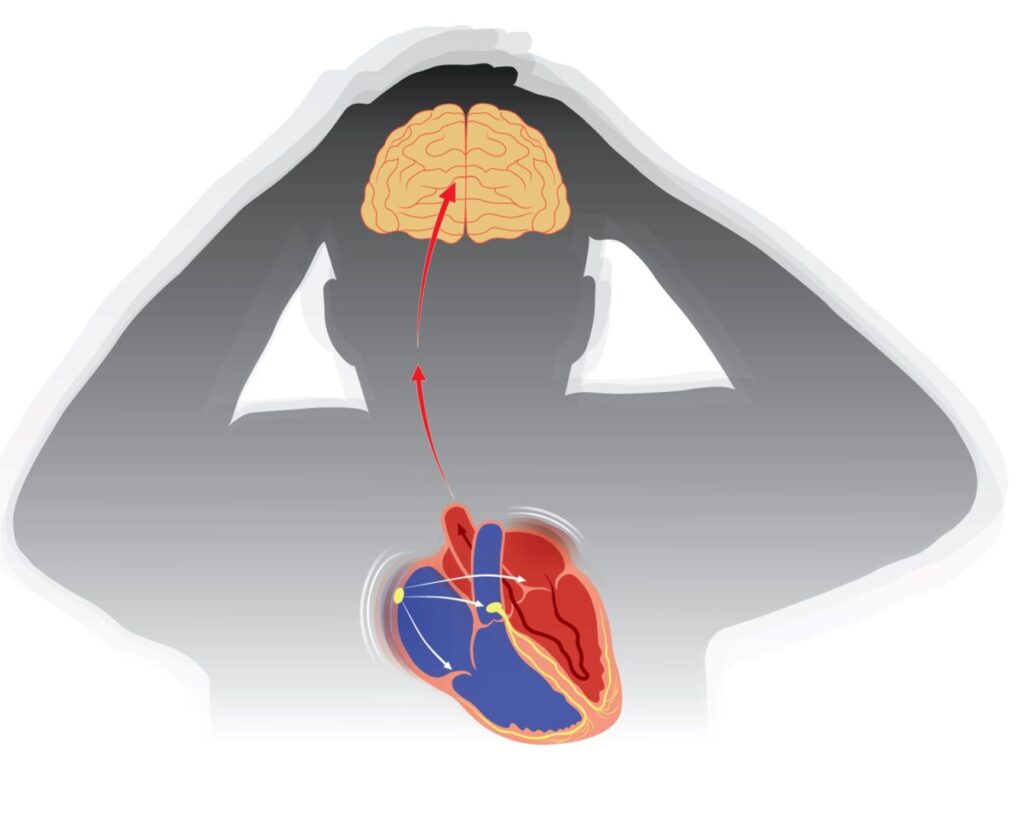
Atrial fibrillation (AFib) is a common type of arrhythmia characterized by an irregular and often rapid heart rate. It occurs when the heart’s upper chambers (atria) beat chaotically and out of sync with the lower chambers (ventricles). This irregular rhythm can lead to poor blood flow, increasing the risk of stroke, heart failure, and other heart-related complications.
The symptoms of atrial fibrillation can vary. Some people experience noticeable symptoms such as heart palpitations, shortness of breath, weakness, fatigue, dizziness, or chest pain, while others may have no symptoms at all. AFib can be occasional (paroxysmal), persistent, or permanent, depending on its frequency and duration.
Several factors can increase the risk of developing AFib, including high blood pressure, heart disease, diabetes, obesity, excessive alcohol consumption, and a family history of arrhythmias. Other risk factors include advancing age, thyroid disorders, and sleep apnea.
Diagnosis involves a combination of medical history, physical examination, and tests such as electrocardiograms (ECG), Holter monitors, and echocardiograms to confirm the presence of AFib and assess its impact on the heart.
Treatment aims to control the heart rate, restore normal rhythm, and reduce the risk of stroke. This may include lifestyle changes, medications like beta-blockers, calcium channel blockers, antiarrhythmics, and anticoagulants to prevent blood clots. In some cases, procedures such as electrical cardioversion, catheter ablation, or the implantation of a pacemaker may be necessary to manage the condition effectively.
Proper management of atrial fibrillation can significantly reduce symptoms, improve quality of life, and lower the risk of serious complications.